A French company is preparing to test a complex artificial heart that combines biology with machinery.
- By Susan Young Rojahn on May 30, 2013
Why It Matters
A lot of people in the world have heart failure, meaning their hearts cannot pump enough blood and oxygen to other organs.
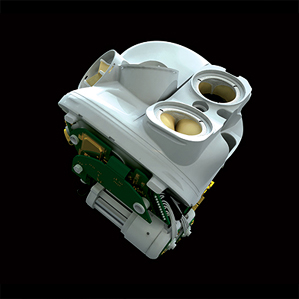
Cardio cyborg: This rendering shows the biological valves at the top of Carmat’s artificial heart.
A new kind of artificial heart that combines synthetic and biological materials as well as sensors and software to detect a patient’s level of exertion and adjust output accordingly is to be tested in patients at four cardiac surgery centers in Europe and the Middle East. If the “bioprosthetic” device, made by the Paris-based Carmat, proves to be safe and effective, it could be given to patients waiting for a heart transplant. Currently, only one fully artificial heart, made by Tucson, Arizona-based SynCardia, has U.S., Canadian, and European regulatory approval for use in patients.
Attempts to completely replace the human heart with a prosthetic device started decades ago (see “CPR for the Artificial Heart”). It is hugely challenging to create a device that can withstand the harsh conditions of the body’s circulatory system and reliably pump 35 million times per year, as the heart does. Other complications, such as stroke caused by blood clots in artificial heart implants, have also caused setbacks. For these reasons, fully artificial hearts typically serve as a temporary measure, or as a “bridge to transplant,” although the FDA has recently granted a humanitarian use exemption for one of SynCardia’s artificial hearts for patients not currently eligible for a donor heart.
But the great need for a life-saving treatment in heart-failure patients has driven investigators, both in academia and private industry, to try to build a better artificial heart. Around 5.7 million people in the U.S. have heart failure at any given time, according to the Centers for Disease Control and Prevention. In these patients, the heart’s pumping abilities have grown so weak that it cannot deliver enough oxygen and nutrients to the body. Sometimes failure is limited to one side of the heart and can be treated with an implant that boosts flow but does not replace the heart entirely. But in cases where both sides of the heart are failing, a patient will need a heart transplant. And with demand for heart transplants far exceeding donations, patients can wait for years for a donor heart, while others may be ineligible altogether because of other health issues.
An artificial heart can provide a life-saving bridge while a patient waits for a transplant. Surgeons have implanted a SynCardia artificial heart in over 1,000 patients. Air is pumped from the external control system (which has recently evolved from a large, 418-pound driver to a wearable 13.5-pound driver) through tubes that connect through the skin into the device. Puffs of air expand two small balloons inside each chamber of the artificial heart, which pushes blood out of the prosthesis.
In Carmat’s design, two chambers are each divided by a membrane that holds hydraulic fluid on one side. A motorized pump moves hydraulic fluid in and out of the chambers, and that fluid causes the membrane to move; blood flows through the other side of each membrane. The blood-facing side of the membrane is made of tissue obtained from a sac that surrounds a cow’s heart, to make the device more biocompatible. “The idea was to develop an artificial heart in which the moving parts that are in contact with blood are made of tissue that is [better suited] for the biological environment,” says Piet Jansen, chief medical officer of Carmat.
That could make patients less reliant on anti-coagulation medications. The Carmat device also uses valves made from cow heart tissue and has sensors to detect increased pressure within the device. That information is sent to an internal control system that can adjust the flow rate in response to increased demand, such as when a patient is exercising.
The system was developed through collaboration between the European Aerospace and Defense Systems and Alain Carpentier, a cardiac surgeon who pioneered heart valve repair.
“It’s a brilliant device; I just worry about the size and mechanical durability,” says William Cohn, a heart surgeon at the Texas Heart Institute in Houston. Tasked with pumping 100,000 times or more a day, most artificial hearts don’t last more than a few years, says Cohn. “A device that lasts two to three years is, at best, a stopgap for transplant.”
Carmat’s device is just one of several artificial hearts in development across the globe. Cohn and colleagues have been testing another sort of artificial heart which does not generate a heartbeat, but instead continuously pumps blood out through the body. The hope is that a continuous-flow heart, although quite different than the natural organ, will avoid the risk of mechanical failure that hangs over the pulsing-flow artificial hearts.
Recently, the Texas Heart Institute recruited Australian engineer Daniel Timms to bring his novel continuous-flow artificial heart to Houston. The device is small, does not pulse, and has a single moving part: a magnetically levitated rotor that sports two impellers, one that pushes blood from the body into the lungs to be re-oxygenated, and the other to push the oxygen-rich blood into the body. The simplicity of the design, which Cohn says should resist mechanical wear and tear, contrasts with the complex Carmat artificial heart, which contains many moving parts. But Timms’s system is years away from being tested in patients, and will first be tested in calves.
Carmat's second patient was implanted on 2014, August 5: Health ministry
PARIS (Reuters) - An artificial heart made by Carmat was fitted into a second patient on Aug 5 and the operation went smoothly, the French health ministry said in a statement on Monday.
"The operation was carried out in good conditions" at the CHU hospital of Nantes, the statement said, adding that the minister sent her best wishes to the patient, of whom no details were given.
Carmat confirmed earlier on Monday it had fitted a second patient with one of its artificial hearts and would continue its clinical trials on two more patients. It did not reveal a date.
The clinical trial be considered a success if these first patients survive with the implant for at least a month. The patients selected suffer from terminal heart failure - when the sick heart can no longer pump enough blood to sustain the body - and have only a few weeks, or even days, to live.
(Reporting by Natalie Huet; Editing by Brian Love)

Nenhum comentário:
Postar um comentário
Observação: somente um membro deste blog pode postar um comentário.